We have tiny visitors that have taken advantage of their evolutionary squatting rights throughout our bodies; these microbes make up our microbiome. Nobel Laureate Joshua Lederberg best defined the human microbiome as “the ecological community of commensal, symbiotic, and pathogenic microorganisms that literally share our body space”.
We are Soylent Microbiome, Soylent Microbiome is US!
This means we have 3 distinct types of microorganisms sharing our bodies with us:

1) The Commensals: Commensalism is relationship between two organisms where one benefits without affecting the other, derived from the English work commensal meaning “eating at the same table”.
2) The Symbionts: This is a clear mutualistic relationship, both parties are benefiting, both parties are happiest. We provide love to our microbiome, they provide love back to us (and by love I mean nutrients and protection from harm).
3) The Pathogens: These are the microbes that cause disease. The main distinguishing factor of a pathogen vs. a commensal is that a pathogen causes harm to the host.
Maintaining the perfect balance of all 3 of these microbe-types is essential for the equilibrium of the microbiome. An altered microbiome has been linked to depression, obesity, diabetes, anxiety, autism, cancer, rheumatoid arthritis, muscular dystrophy, multiple sclerosis, fibromyalgia and many other negative aspects of being human that we have yet to link.
We know one sure-fire way to disrupt the gut microbiome is to treat a human with oral antibiotics. Yes, the cure for most bacterial infection is to wipe out your entire ecological masterpiece you’ve worked on for decades in your gut.
Essentially, your commensals and symbionts work together to protect you from the potential harm that can be caused by the pathogens. We don’t understand fully how the protection works, but we do know that the presence of commensals and symbionts are essential for keeping the pathogens at bay.
One hypothesis is that your commensals and symbionts are creating a literal barrier between you and the pathogens, and if you wipe out this barrier with antibiotics that is when the scary pathogens take over.
In fact, oral antibiotic use is one of the leading risk factors for the disease associated with Salmonella ssp. and Clostridium difficile (C diff).
In most cases, Salmonella spp. causes salmonellosis (or food poisoning) and typhoid fever, whereas C. difficile causes antibiotic-associated diarrhea (AAD). In more severe cases Salmonella spp. can cause sepsis and C. difficile can cause “pseudomembranous colitis”, a severe inflammation of the colon.
But back to our story! The key is to keep these pathogens quiet and happy, and if oral treatment with antibiotics disrupts the microbiome barrier that leads to these pathogens causing disease and harm…
WHAT IS IT ABOUT THE DISRUPTION OF THE MICROBIOME BY ANTIBIOTICS THAT BENEFITS THE PROLIFERATION OF THE PATHOGENS?
Turns out, sugar availability is at an all-time high for these pathogens when the microbiome is disturbed, specifically an increase in sialic acid (yum!) and fucose (yummier!).
The mammalian host is nutrient diverse and rich, allowing for microbial populations to snuggle up and settle in – however the intestinal microbial community (or the microbiota) is composed of trillions of bacterial cells, making nutrient availability a little more stringent for those invaders that try to squat in the gut.
Alteration of the microbiome leads to an alteration of the carbohydrate availability in your gut – and the pathogens that are now rattled by the disruption of the microbiome now have unlimited food.
More sugar = more replication = more disease
Think of Salmonella spp. and C. difficile as Scrooge McDuck rolling around in his pile of money.
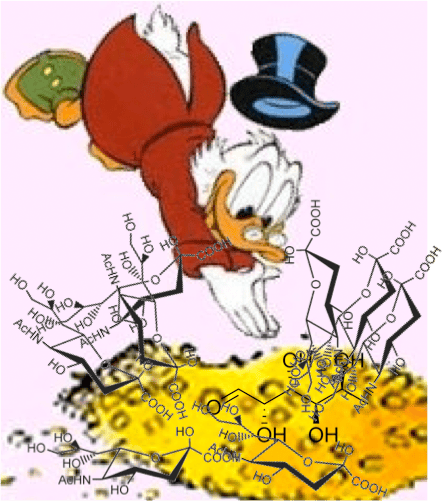
Katherine Ng in Justin Sonnenburg’s lab at Stanford University found that during oral treatment of antibiotics there is a spike in microbiota-liberated sugars that can then be taken up and eaten by our protagonists, Salmonella spp. and C. difficile to increase their replication and disease in the gut.
Specifically, Salmonella spp. are utilizing the liberated sialic acids and fucose from disturbed commensals in the gut after antibiotic treatment, and C. difficile is utilizing the the sialic acids liberated by the same commensals.
Interestingly, when you delete these catabolic pathways (metabolic pathways in the bacteria that are used to break down molecules into smaller units for energy) in Salmonella spp. where it can no longer use sialic acid and fucose as carbon sources, it can no longer replicate and cause disease to the same levels in antibiotic-treated mice.
Not only that! When you have a mouse with a microbiome that cannot produce sialic acid, therefore it reduces free sialic acid levels, C. difficile no longer causes disease to the same levels after treatment with antibiotics. No free sugars? No good for our protagonists!
What if we took these mice that had a microbiome that does not produce sialic acid and we fed them sialic acid in their diet (nom nom), then we treated the mice with antibiotics = C. difficile reigns again!
It looks like that usually, when the microbiome is happy, it’s eating all the free sialic acid and fucose and not saving any for the pathogens, which keeps the pathogens at a minimum and less of a nuisance – however, upon antibiotic treatment the microbiome is disturbed, which breaks down the wall of commensal/symbionts blocking pathogens from using these sugars… therefore the pathogens are eating good, replicating, and eventually cause disease.
Pathogens, always the opportunists.
HOW CAN WE USE THIS INFORMATION FOR GOOD?
CAN WE USE THIS INSIGHT FOR NEW THERAPEUTIC APPROACHES TO PREVENTING DISEASES CAUSED BY ANTIBIOTIC-ASSOCIATED PATHOGENS?
During treatment with oral antibiotics what if modulated diet to decrease sialic acid and fucose? Decreasing the availability for pathogens in the gut?
What if we could give a probiotic that was deficient in sialic acid and fucose production, therefore it would be established in the gut and if/when antibiotic are used and disturb the microbiome there would be minimal free sialic acid and fucose because there was none to begin with?
What if we designed an inhibitor that blocked sialic acid and fucose catabolism pathways in the pathogens? Therefore, when antibiotics are used and disrupt the microbiome allowing for pathogens like Salmonella spp. and C. difficile to replicate – we treat with this inhibitor of sialic acid/fucose catabolism, essentially the pathogens could then pick up the sialic acid and fucose from the environment but they couldn’t use is for energy. No energy = no replication = no disease.
Those are just a few of my ideas. What about you?